Given the breadth and magnitude of vaccine safety activities, it is surprising how wide the belief is that the world relies on voluntary reports of adverse events, even among health professionals. That this science is so misunderstood provides fertile ground for anti-vaccine messages to propagate. The safety of vaccines is established using many approaches throughout the life of the product and often beyond. Safety studies take place across the globe and are undertaken by a range of agencies from regulatory to academic to research institute to industry. Here is some information to help challenge the misconceptions.
Voluntary reporting of adverse events after a medicine including vaccines are important
Voluntary/passive/spontaneous – pick your adjective, they all mean much the same when it comes to pharmacovigilance. Such systems exist in most countries and serve to collect reports of possible drug reactions. It may be counterintuitive to know that in the world of pharmacovigilance, a good system receives many reports per 100,000 people in the population. This is not because the medicines are dangerous but because the community are good at reporting adverse events that occur after receipt of a medicine. The reason this is considered good is because it can lead to the detection of safety signals of concern.
It does not mean that all the events reported have been caused by said medicine. Correlation is not the same as causality and the error in thinking is called post hoc ergo propter hoc, which is Latin for after this, therefore because of this.
Understanding the background rates of different health conditions can be useful as this provides us with what we should expect to see following vaccination by chance. (PMCID7936550)
Voluntary reporting of adverse events after immunisation does not mean the vaccine caused the event but reports are often misused
A common misunderstanding is that all reports of adverse events received have been caused by the receipt of a vaccine, the post hoc fallacy. The data collected in this way has been used for years by disinformation merchants and it is perhaps one of the most common tropes among the anti-vaccine community to report the numbers of deaths and other serious events as if caused by vaccines and the language used is provocative.
Sen. Ron Johnson (R-Wis.): “Well, I can report what’s being reported on the VAERS system. … It’s an imperfect system. In general, the complaint is a very small percentage of adverse effects actually get reported, and so you have to take this with a grain of salt, but according to the VAERS system, we are over 3,000 deaths of, after, within 30 days of taking the vaccine. About 40 percent of those occur on Day Zero, One or Two.”
— Exchange on “The Vicki McKenna Show,” May 6, 2021
A recent, quite elaborate, example of the use of passively reported data is via information obtained through the US Freedom of Information Act to acquire all data provided by Pfizer in support of the vaccine registration. One document is a report of adverse events the company have been made aware of through passive reporting systems. This report has been framed as
“Safety surveillance data in the Pfizer’s document shows harmful effects of the Pfizer-BioNTech COVID-19 vaccine.”
No, it does not, and this is misleading at best. The safety surveillance data in the document do not show that the vaccine caused the reported events or that the vaccine is unsafe for the reasons described above.
How vaccine safety is actually assessed
If we relied solely on people voluntarily reporting adverse events that occurred after receiving a vaccine, we would not know:
- How many of the events were caused by the vaccine (if any) and how many were coincidental events
- What the real risk from the vaccine is if any
This would be problematic because it would make decisions on use very difficult, we would be flying blind. To address these two vital questions, the following approaches are used, usually in this order:
1. Determine if there are more observed events than are normally expected. One way is to look at the regular rates of hospitalisation for the event of concern before the vaccine was used and see if the rates went up after the introduction of the vaccine. If there are more than normally expected, then you have a safety signal. Here is an of what this might look like.
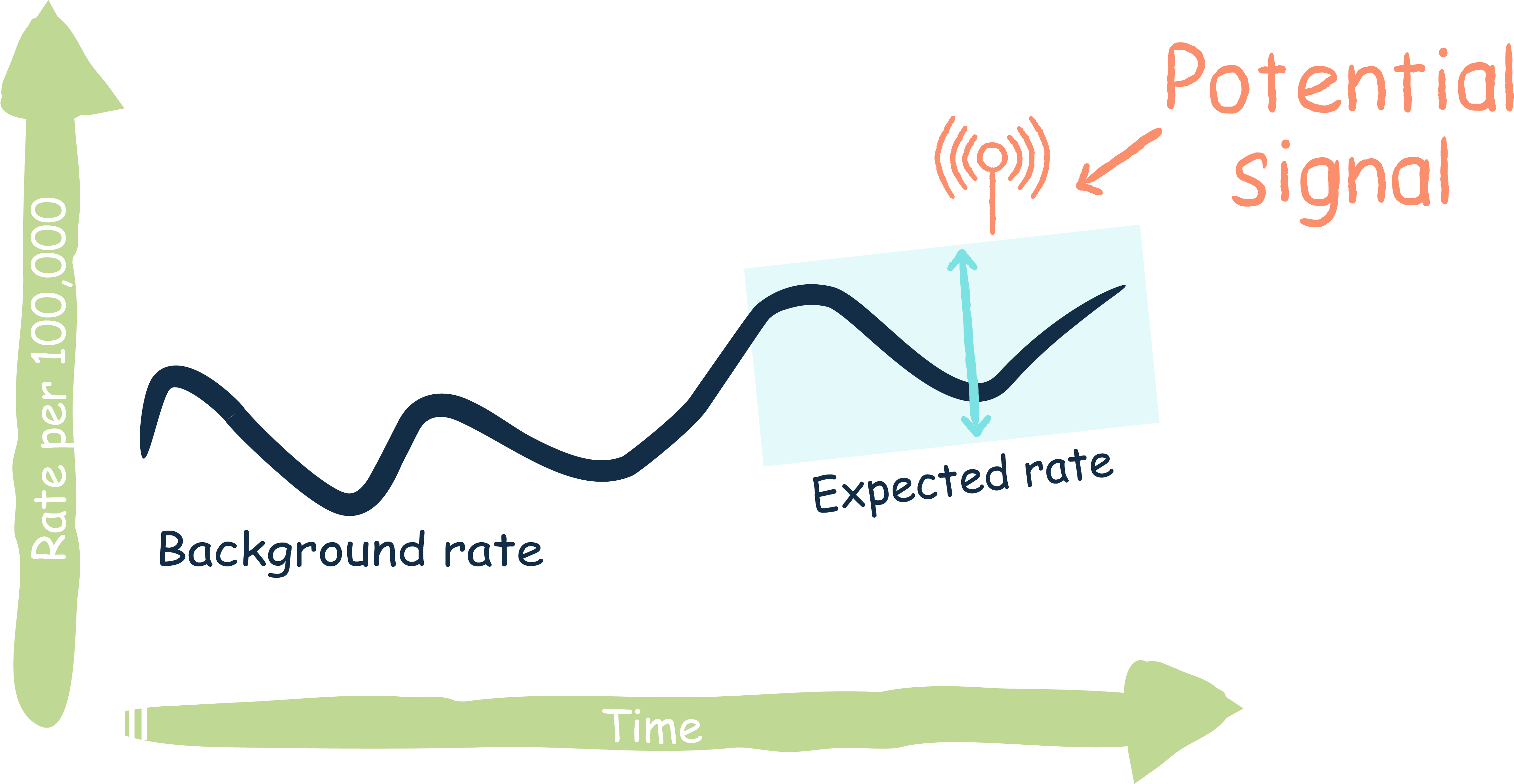
2. The above diagram depicts a safety signal. To investigate a safety signal there are a range of methods, but they all share the common feature of comparing vaccinated people with unvaccinated people. For example, one might find all hospitalisations for a certain condition then look at the vaccine status of the cases. In some countries this can be done for the entire population, so can often include millions of people. Here are some examples with links:
- Andrews NJ, Stowe J, Ramsay MEB, Miller E. Risk of venous thrombotic events and thrombocytopenia in sequential time periods after ChAdOx1 and BNT162b2 COVID-19 vaccines: A national cohort study in England. Lancet Reg Health Eur. 2022;13. PMID34927118
- Barda N, Dagan N, Ben-Shlomo Y, Kepten E, Waxman J, Ohana R, et al. Safety of the BNT162b2 mRNA Covid-19 vaccine in a nationwide setting. N Engl J Med. 2021. PMID33626250
- Dodd CN, Romio SA, Black S, Vellozzi C, Andrews N, Sturkenboom M, et al. International collaboration to assess the risk of Guillain Barré Syndrome following Influenza A (H1N1) 2009 monovalent vaccines. Vaccine. 2013;31(40):4448-58. PMID23770307
- Klein NP, Lewis N, Goddard K, Fireman B, Zerbo O, Hanson KE, et al. Surveillance for adverse events after COVID-19 mRNA vaccination. JAMA. 2021. PMID34477808
- Stock SJ, McAllister D, Vasileiou E, Simpson CR, Stagg HR, Agrawal U, et al. COVID-19 in Pregnancy in Scotland (COPS): protocol for an observational study using linked Scottish national data. 2020;10(11):e042813. PMID 3324817
There are many variations on the above two themes that researchers can, and do, use to evaluate vaccine safety. The results from such investigations contribute to the overall understanding of vaccine safety and help inform important decisions, such whether to withdraw a vaccine or restrict its use.
Using multiple methods of assessment of vaccines, we have established that the Pfizer/BioNTech mRNA is very safe and serious adverse events are very rare. The only serious event for which the risk has been found to be increased after the vaccine is inflammation of the heart (myocarditis or pericarditis). The risk appears to be highest for younger males. We understand this risk not from passive reporting, where cases could be missed and data are often incomplete, but from active investigations that search for the cases. COVID-19 disease itself carries far more risk of severe heart inflammation as well as other severe effects.
Summary of approaches to post marketing vaccine safety monitoring
Mitigating damage from misinformation
The ongoing dissemination of false and misleading claims about vaccine safety issues using data from passive safety surveillance systems continues to impact on the efforts to control not only the COVID-19 pandemic but also other infectious diseases. Serious side effects from authorised vaccines are extremely rare, modern technologies and methods play an important role in understanding them.
Here are three tips for mitigating some of the damage from misinformation with further reading and guidelines provided below.
1. Challenge vaccine safety misinformation by effective debunking
a. Lead with the facts (keep them simple and sticky).
b. Warn about the myth (just once).
c. Expose the manipulation technique – explain why the myth is misleading such as the post hoc fallacy above.
d. End by reinforcing the facts to provide a credible alternative explanation.
2. Prebunk
a. Help people understand that vaccines are monitored in many ways to create a ‘body of evidence’.
b. Forewarn people about impending vaccine misinformation and tell them how to spot it. This generates ‘cognitive’ antibodies that effectively inoculate people against misinformation.
Further useful resources
- Black SB, Law B, Chen RT, Dekker CL, Sturkenboom M, Huang W-T, et al. The critical role of background rates of possible adverse events in the assessment of COVID-19 vaccine safety. Vaccine. 2021;39(19):2712-8. PMCID7936550
- Lewandowsky S, Cook J, Ecker UKH, Albarracín D, Amazeen MA, Kendeou P, et al. The Debunking Handbook 2020 [Internet] 2020. Available from: https://sks.to/db2020
- van der Linden S. Misinformation: susceptibility, spread, and interventions to immunize the public. Nat Med. 2022;28(3):460-7. PMID 35273402
Photo credit, spiral staircase: Magdalena Roeseler, CC BY 2.0, via Wikimedia Commons.

